Every child deserves a chance at life, yet for thousands in India suffering from severe liver diseases, this chance is often out of reach. A staggering reality—only 1 in 10 children in need of a liver transplant receives one. Behind these numbers are families grappling with not just the emotional turmoil of seeing their child suffer, but also the insurmountable financial and logistical barriers that stand in the way of life-saving treatment.
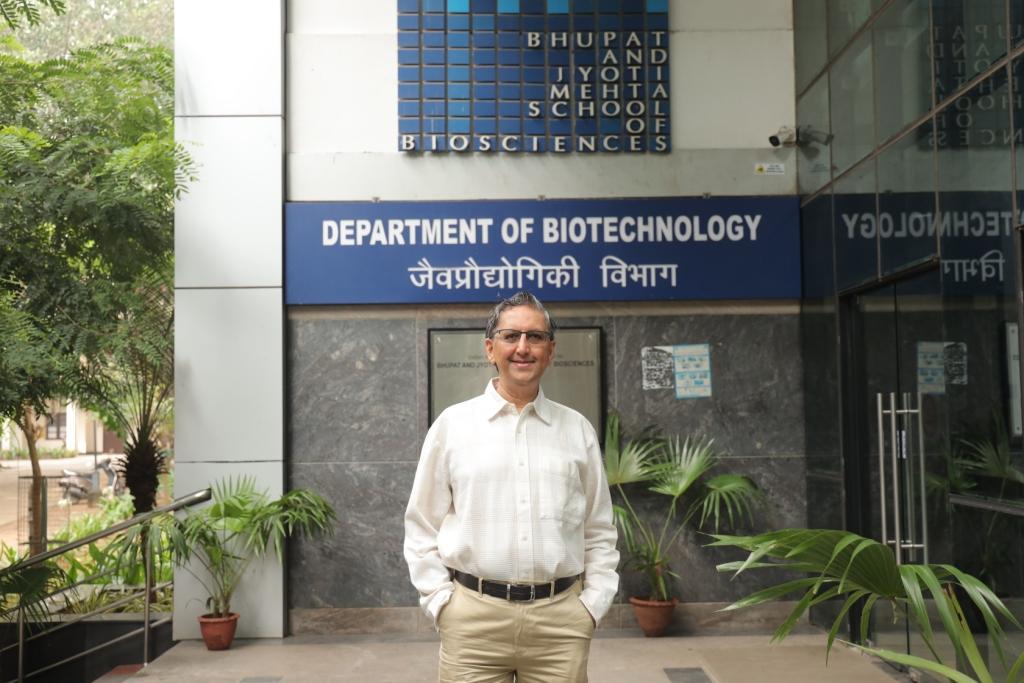
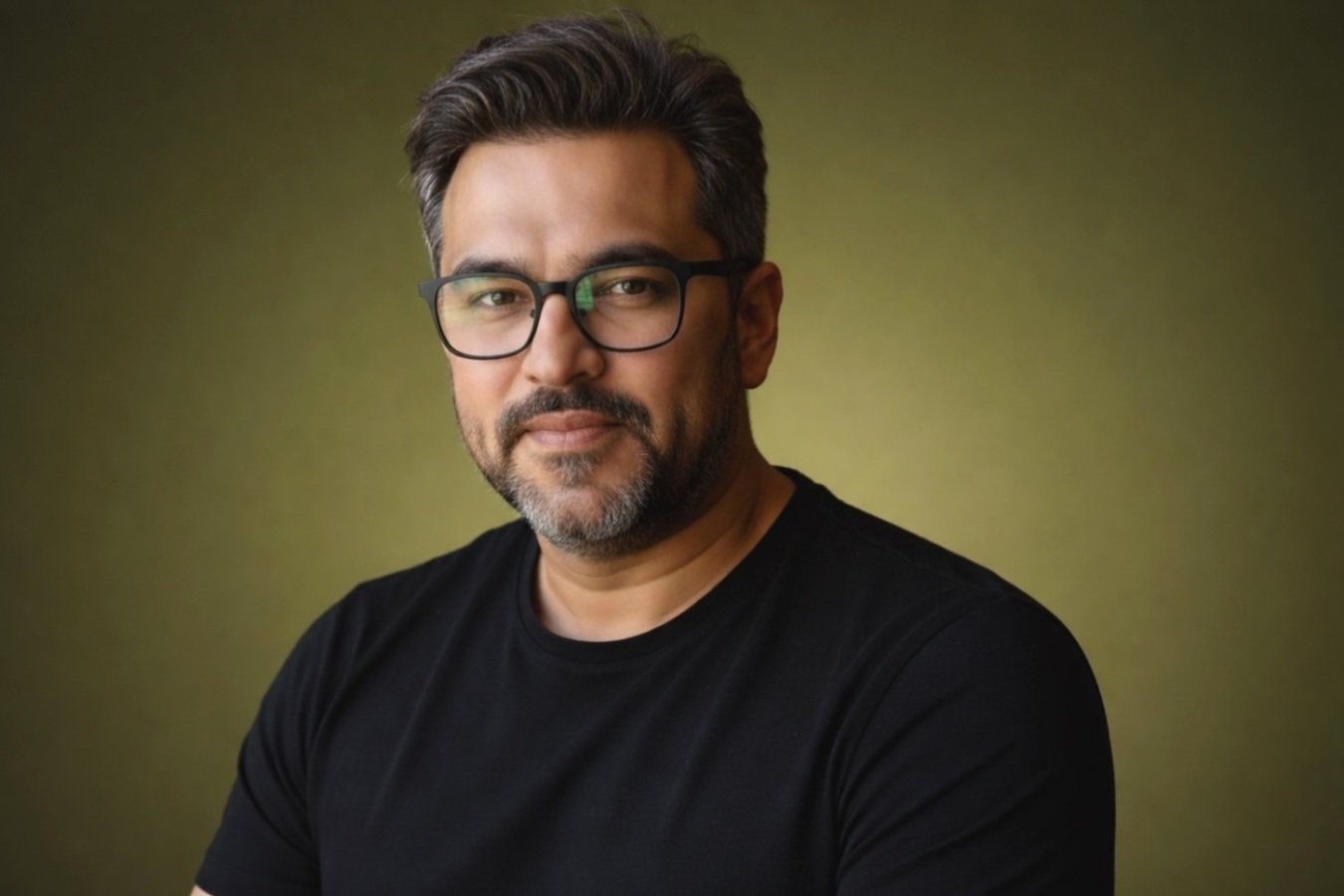
For Mr. Pravin Agarwal, Vice Chairman and Whole-time Director of STL (Sterlite Technologies Limited), this was not just a statistic—it was a call to action. The Pravin Agarwal Foundation (TPAF) was born out of a deep-seated conviction that no child should be denied a future due to a lack of resources. Since its inception, TPAF has played a crucial role in supporting liver transplants for children in need, enabling hundreds of successful procedures and giving them a new lease on life. By bridging gaps in affordability, accessibility, and awareness, TPAF is ensuring that life-saving transplants are no longer a privilege but a possibility for children across India. Through innovative financial aid programs, collaborations with hospitals, and ecosystem-wide interventions, the foundation is making a lasting impact on pediatric liver transplant care.
In this exclusive interaction with TheCSRUniverse, Mr. Agarwal sheds light on the pressing challenges of pediatric liver transplants, the foundation’s pioneering initiatives, and the human stories that fuel their mission. This is more than a conversation; it’s a testament to the power of compassion, collaboration, and the belief that one life saved can transform many more.
Scroll down to read the full interview.
Q&A
Q. What motivated you to establish The Pravin Agarwal Foundation (TPAF) with a focus on pediatric liver transplants? What are the key challenges families face in accessing this life-saving treatment, and how does TPAF address these through its financial assistance programs?
A. Passion is a powerful feeling that commands one's interest and fuels the desire to make a meaningful contribution. TPAF was born from Mr. Pravin Agarwal's lifelong desire to improve the world. The focus on pediatric liver transplants arose from a stark realization: only one in ten children needing a liver transplant receives one. This dire gap between demand and supply, revealed through research and hard facts, spurred action.
Pediatric liver transplantation is a highly specialized area, demanding significant expertise, substantial financial investment, extensive geographical reach, and widespread public awareness. The absence of dedicated thought leaders to champion this cause served as a powerful impetus for the foundation to pursue this mission with unwavering conviction.
The simple idea that enriching one child's life positively impacts their family and community highlights the compounded good and significant impact of this work. Furthermore, the fact that parents are typically the liver donors creates a powerful sense of rebirth, transparency, and credibility in an often-controversial field of organ transplantation.
TPAF pursues this cause with unwavering conviction, making it a deeply meaningful part of the lives it touches.
Challenges:
Living Donor Availability – Pediatric liver transplants primarily rely on living donors, usually a family member. However, convincing non-related adults to donate remains a challenge due to a lack of awareness.
Deceased Organ Donation Rates – While medical advancements allow liver transplants from deceased donors, persuading families to consent to donation remains difficult, leading to a severe shortage.
Time Sensitivity – Liver transplants are highly time-sensitive, especially for newborns and young children with weaker immunity. The lack of an organized system for timely donor organ procurement adds to the challenge.
Financial Barriers – Despite being relatively affordable in India compared to other countries, liver transplants remain out of reach for many families. Limited health insurance coverage and difficulty in accessing financial aid further complicate matters.
Post-Transplant Care and Rejection Risks – Even after a successful transplant, children require lifelong immunosuppressive medication and regular medical follow-ups. However, due to financial constraints, many families struggle to afford these essential medicines, leading to increased risks of organ rejection.
Awareness and Early Diagnosis – Diseases like Biliary Atresia, a leading cause of pediatric liver failure, require early intervention. Many parents and even healthcare providers are unaware of early symptoms, leading to delayed diagnosis and reduced chances of successful treatment.
TPAF’s Financial Assistance Programs:
Affordable Liver Transplant Program – This program is solely aimed at children, from ages new born to 17 years who are due to receive a liver transplant. The nationality of such children may however vary. There are over 15 Hospitals across India which actively refer such cases to TPAF for fund assistance and perform the transplants. Currently, TPAF has supported patients from hospitals in Maharashtra, Delhi, Karnataka, Kerala, Haryana, Tamil Nadu and Telangana.
Biliary Atresia Support Program – Biliary Atresia (BA) is a congenital, progressive, sclerosing disease of the biliary tracts of a new born infant. It is the top indication for a liver transplant in children. In the absence of appropriate treatment, these children rapidly develop liver failure and do not survive beyond their second birthday. The optimal initial procedure is an operation called Kasai Portoenterostomy (KPE). This procedure, if done within 60 days of life, preserves liver function in about 60 to 70% children for many years. TPAF enables KPE for children suffering from Biliary Atresia as an intervention to prevent or delay the need for Liver transplantation in these children. A successful KPE procedure pushes the requirement of liver transplantation(LT) by many years and even decades- at which time transplantation is safer and has better outcomes.
Q. Collaborations play a vital role in addressing healthcare challenges. How have TPAF’s partnerships with NGOs, medical institutions, and crowdfunding platforms contributed to easing the financial burden of pediatric liver transplants? Can you share successful examples and key learnings for future partnerships?
A. Through the Foundation, we have established a unique ecosystem involving hospitals, highly qualified doctors and crowd funding platforms and funding/ grant-giving organisations to enable access to affordable liver treatment for children. Our collaborative and agile methodology allowed us to distribute the costs of liver transplant, reduce turnaround time for raising funds and allowed families of affected children to get a greater leverage in engaging with healthcare administrators to reduce costs of liver transplant surgeries. A targeted, systematic eradication of a seemingly-insurmountable challenge is easier, scalable and ultimately more impactful when you join hands with the right partners.
In cases where crowdfunding has fallen short of the requisite budget for liver transplant, TPAF has stepped in to address the funding and insurance gap. More than the financial aid, the model has served to foster greater community action and galvanised efforts of individuals and institutions from different quarters.
Success Stories:
Badukonda’s Journey – A six-year-old from Andhra Pradesh diagnosed with liver failure. TPAF collaborated with his parents, a crowdfunding partner, and Rela Hospital, where he underwent a successful liver transplant.
Asdak’s Fight Against Wilson’s Disease – A nine-year-old diagnosed with Wilson’s Disease required a liver transplant. TPAF supported him from fundraising to surgery and recovery.
The success stories of these children have given us a new hope that we are on the correct path and have enabled us to build traction and scale to support many more children in need of liver transplant. Since our inception in 2016, we have supported nearly 500 paediatric liver transplants across India.
Q. Given the importance of specialized expertise in pediatric liver transplants, how is TPAF working to strengthen medical networks and training programs for healthcare professionals? How do you measure their impact, and are there plans to establish regional centers of excellence?
A. TPAF has facilitated ecosystem-level change by partnering at conferences for liver transplantation surgeons, paediatricians and transplant coordinators to raise awareness regarding the availability of funding for paediatric liver transplantations. TPAF has hosted annual roundtables to initiate dialogue amongst key players in paediatric liver transplantation ecosystem - expert doctors, healthcare professionals, philanthropists, foundations, and crowdfunding partners - to increase to be able to support more children in need. Measuring and communicating our impact is crucial to our success. We have implemented robust monitoring and evaluation frameworks to assess the effectiveness of our programs, measure outcomes and identify areas for improvement. Our communication strategies will be enhanced to regularly share our progress, successes, and challenges with stakeholders, ensuring transparency and accountability.
Q. Early diagnosis of Biliary Atresia is crucial for better transplant outcomes. What specific initiatives has TPAF undertaken to raise awareness among communities and healthcare providers, and what strategies are being used for effective information dissemination?
A. Biliary Atresia support program aims to:
- Identify children with Biliary Atresia children within the 3rd or 4th week of life.
- Ensure timely referral and resources for children with Biliary Atresia to be optimised and offered Kasai portoenterostomy within the 60 day period.
- Standardize preoperative preparation of children before KPE
- Standardize the surgical procedure of KPE
- Standardize post operative care and use of specific medications after the KPE to achieve optimal success.
- Identify children requiring liver transplantation when KPE is unsuccessful. This will help optimization of their health, prolong their native liver survival and decrease the need for early transplantation.
To achieve these goals, we target interventions at various levels:
- Neonatologists, pediatricians, and rural healthcare workers – To improve early detection and referrals.
- Pediatric surgeons and gastroenterologists – To standardize surgical and post-operative care.
- Public education campaigns – Inspired by initiatives like the UK’s "Yellow Alert," where parents and primary care doctors monitor newborns' stool color as an early indicator.
Overall these intervention should result in the following measurable goals:
- Neonatologists, pediatricians, and rural healthcare workers – To improve early detection and referrals.
- Pediatric surgeons and gastroenterologists – To standardize surgical and post-operative care.
- Public education campaigns – Inspired by initiatives like the UK’s "Yellow Alert," where parents and primary care doctors monitor newborns' stool color as an early indicator.
Q. Post-transplant care is critical, yet many families struggle with distance and financial constraints. How can technology, such as telemedicine, help address these challenges? Are there any technology-driven initiatives TPAF is pursuing?
A. By definition, telemedicine refers to the remote diagnosis and treatment of patients through telecommunication technologies. This mode of treatment is rapidly being embraced by the medical fraternity. In fact, it is believed that since telemedicine is a convenient and cost-effective method of treatment, in-person visits for post-transplant care should become a second, third, or even last option for meeting a patient’s needs.
Telemedicine helps protect vulnerable individuals, such as transplant recipients and donors, by limiting their contact with other patients and healthcare staff. Additionally, it benefits families by reducing the financial burden associated with frequent hospital visits. This approach minimizes non-medical out-of-pocket expenses, including travel, accommodation, loss of work, and other related costs.
Q. How does TPAF measure the success and impact of its programs, both short-term (e.g., successful transplants) and long-term (e.g., quality of life)? Could you share specific success stories or impact numbers that illustrate the Foundation’s work?
A. Measuring and communicating our impact is crucial to our success. We have implemented robust monitoring and evaluation frameworks to assess the effectiveness of our programs, measure outcomes and identify areas for improvement. Our communication strategies periodically enhanced to regularly share our progress, successes, and challenges with stakeholders, ensuring transparency and accountability.
Since 2016, TPAF collects information from the partner hospitals to understand the landscape of and critical challenges surrounding pediatric liver transplants in the India. TPAF also routinely connects telephonically with parents of children who were financially supported by TPAF for their liver transplant. Over 98% parents were satisfied with their child’s health post-transplant, which demonstrates the transformative impact of this unique medical intervention. An increase in child's physical activity after the transplant was reported by 79% parents, of which 74% shared that their child engaged in any form of physical activity on a daily basis. It shows that a liver transplant has an overall positive impact on the life of the child and his family.
Q. Given your leadership roles at STL and Sterlite Power Transmission—companies focused on infrastructure—how do you view the role of public-private partnerships in strengthening healthcare infrastructure? Specifically, how can these partnerships bring life-saving treatments like pediatric liver transplants closer to underserved regions? What role do businesses play in bridging this critical gap?
A. Public-Private Partnerships have immense potential in various regions across the country. Through such collaborations, corporate doctors can perform pediatric liver transplants in government facilities, helping build the facility’s capability by training residents and enhancing its capacity to manage post-transplant care. Additionally, there is a need to drive advocacy movements that push for the government to prioritize the treatment of rare diseases through appropriate budget allocations.
Businesses can play a crucial role in strengthening the pediatric liver transplant ecosystem by initiating legacy-building programs, investing in infrastructure such as advisory services, research, and capacity-building initiatives, and leveraging their influence to encourage peer organizations to support children with rare liver diseases.
Q. As we look toward 2025 and beyond, what are the key focus areas for India's healthcare sector to improve access to life-saving treatments like pediatric liver transplants? What is TPAF’s vision for scaling its impact, and how do you plan to ensure that more children in remote and underserved areas benefit from these critical healthcare interventions?
A. As TPAF looks to the future, our unwavering commitment to creating a comprehensive ecosystem focused on liver disease management for children guides our strategic direction. To amplify our impact and better serve our stakeholders, we have developed a plan to scale up key activities that align with our organizational goals. Our future efforts will concentrate on expanding program offerings, strengthening community engagement, promoting innovation, and enhancing communication to ensure measurable outcomes.
Building on the success of our current initiatives, we plan to broaden our program offerings by extending their scope and reach through advanced methodologies, expanding target audiences, and integrating continuous feedback mechanisms. A particular focus will be on developing new programs that address critical needs within our community, such as the early detection and cost-effective treatment of biliary atresia.
Strengthening community engagement remains central to our mission. We will deepen and nurture partnerships with local organizations, medical institutions, and industry bodies to foster collaboration and resource-sharing. These partnerships are essential for enhancing our collective impact and achieving shared goals more effectively.
Innovation and adaptability are also key to our strategy. We are committed to adopting emerging technologies to streamline our operations, enhance program delivery, and improve stakeholder engagement. Additionally, we are developing flexible planning frameworks that allow us to quickly adapt to changing circumstances, emerging trends, and new opportunities, ensuring that we remain relevant and effective.
TPAF is poised for significant growth and a wider reach in the coming years. By intensifying our efforts in these strategic areas, we aim to strengthen our foundation, expand our impact, and deepen our influence within the community. Our plans are designed to ensure that we continue to fulfill our mission, adapt to evolving needs, and create lasting positive change. We are excited about the journey ahead and remain dedicated to making a meaningful difference through our enhanced efforts and collaborative spirit.












.jpg)